1. Why a Standardized Approach to Dyspnea Matters
This article will provide a clear, systematic approach to dyspnea for clinicians on the front lines.
Dyspnea (shortness of breath) represents one of the most challenging clinical presentations in emergency medicine, primary care, and hospital settings. Each year, nearly 4 million emergency department visits result from respiratory distress, making this one of the most common chief complaints, particularly among elderly patients 11. The sensation of breathlessness arises from a complex interplay between physiological mechanisms and psychological factors, creating a symptom that demands both urgent attention and systematic evaluation 17.
As a clinician, approaching a dyspneic patient requires both rapid assessment skills and methodical clinical reasoning. The experience of dyspnea encompasses at least three qualitatively distinct sensations: air hunger (primal warning of insufficient ventilation), effort to breathe (increased respiratory muscle activity), and chest tightness (often signaling airway constriction). Understanding these distinct sensations provides crucial diagnostic clues that should guide your clinical evaluation.
2. Initial Assessment: The ABCDE Framework
When facing a dyspneic patient, your first priority is determining stability versus instability using the ABCDЕ framework 1:
- Airway: Assess for patency and protection. Listen for stridor (suggesting upper airway obstruction), examine for oropharyngeal swelling, and check for foreign bodies.
- Breathing: Evaluate respiratory rate and oxygen saturation. Rates <10 or >20 breaths/minute or saturation <90% require immediate intervention.
- Circulation: Check for perfusion signs like cyanosis, pallor, or delayed capillary refill.
- Disability: Assess mental status; confusion or inability to speak in complete sentences signals impending respiratory failure.
- Exposure: While respecting privacy, ensure complete examination for clues like edema, rashes, or trauma.
Red flag findings demanding immediate intervention include:
- Use of accessory muscles (scalenes, intercostals)
- Paradoxical breathing patterns
- Inability to speak in complete sentences
- Altered mental status or agitation
- Hemodynamic instability 1
Table: Emergency Findings in Dyspneic Patients and Immediate Actions
| Finding | Possible Cause | Immediate Action |
|---|---|---|
| Stridor | Upper airway obstruction | Airway management, consider epinephrine, steroids |
| Silent chest | Severe asthma/COPD | Nebulized bronchodilators, consider intubation |
| Asymmetric breath sounds | Pneumothorax | Needle decompression if tension suspected |
| Tracheal deviation | Tension pneumothorax | Immediate needle decompression |
| S3 gallop, jugular venous distension | Heart failure | Diuresis, afterload reduction, nitrates |
3. Clinical History: Key Questions and Their Diagnostic Significance
Beyond the immediate assessment, a targeted history provides the most valuable diagnostic information. Focus your questions on these critical areas:
- Onset and duration: “Did your breathing difficulty start suddenly or gradually?”
- Sudden onset: Suggests pulmonary embolism, pneumothorax, aspiration, or anaphylaxis
- Gradual progression: More typical of pneumonia, heart failure, or COPD exacerbation 11
- Positional variation: “Is your breathing worse when lying flat?”
- Orthopnea: Strongly suggests heart failure or diaphragmatic weakness
- Platypnea (worse when upright): Rare but may indicate hepatopulmonary syndrome
- Associated symptoms:
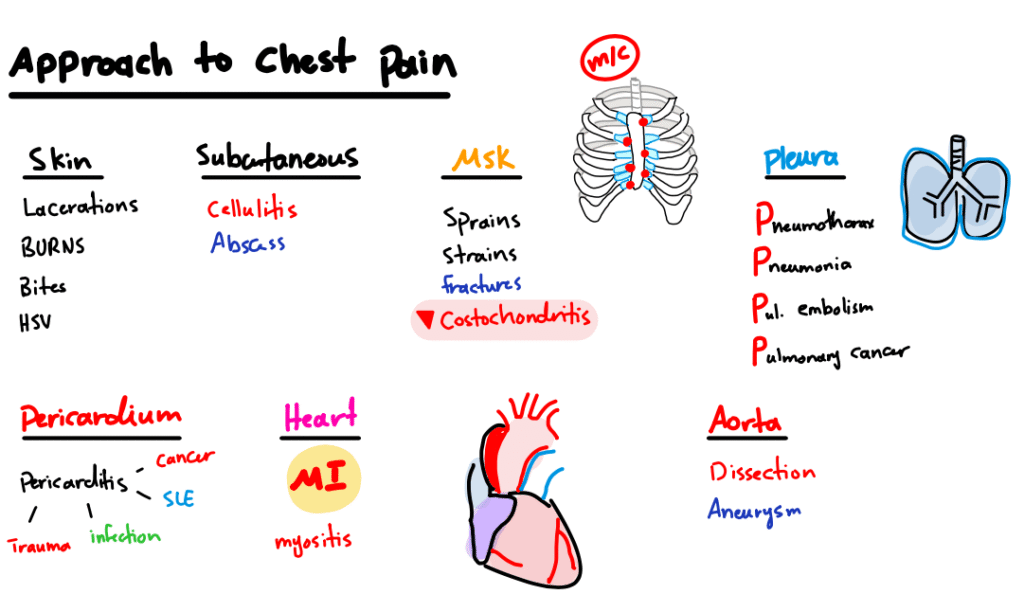
- Chest pain (pleuritic vs. pressure-like)
- Cough (productive vs. nonproductive)
- Fever (suggesting infectious etiology)
- Edema (supporting heart failure diagnosis) 2
- Risk factors:
- Smoking history (COPD, lung cancer risk)
- Occupational exposures (asbestos, silica)
- Travel history (pulmonary embolism risk factors)
- Cardiac history (previous MI, heart failure)
4. The Dyspnea Pyramid: A Visual Diagnostic Framework
Want a Free High-Resolution Copy of This Sketch?
Download the full-size, print-ready PDF of the Dyspnea Pyramid to use as a study aid or quick clinical reference! It’s completely free.
4.1 Cardiac Causes
Cardiac etiologies typically present with signs of volume overload or poor perfusion:
- Heart failure (both systolic and diastolic dysfunction)
- Acute coronary syndromes (myocardial infarction, unstable angina)
- Arrhythmias (atrial fibrillation, tachyarrhythmias)
- Valvular disorders (especially mitral stenosis, aortic regurgitation)
- Pericardial disease (tamponade, constrictive pericarditis)
Diagnostic clues: Elevated BNP/NT-proBNP, S3 gallop, jugular venous distension, peripheral edema, rales on auscultation 11.
4.2 Pulmonary Causes
Pulmonary causes represent the largest category and require careful differentiation:
- Airway diseases: Asthma, COPD, foreign body aspiration
- Parenchymal diseases: Pneumonia, interstitial lung disease, cancer
- Vascular disorders: Pulmonary embolism, pulmonary hypertension
- Pleural diseases: Pneumothorax, pleural effusion
- Restrictive defects: Kyphoscoliosis, massive obesity
Diagnostic clues: Wheezing (obstruction), rales (consolidation or edema), absent breath sounds (effusion or pneumothorax), clubbing (chronic hypoxia) 12.
4.3 Hematologic and Systemic Causes
These often-overlooked categories can present with dyspnea without other respiratory findings:
- Anemia (decreased oxygen-carrying capacity)
- Metabolic acidosis (Kussmaul breathing in DKA, renal failure)
- Systemic disorders (sepsis, anaphylaxis, thyrotoxicosis)
- Toxic exposures (carbon monoxide, methemoglobinemia)
Diagnostic clues: Pallor (anemia), fruity breath (DKA), history of exposure (toxic causes) 2.
4.4 Neuromuscular Causes
These disorders affect the ventilatory pump rather than gas exchange:
- Neurological disorders: ALS, myasthenia gravis, Guillain-Barré syndrome
- Muscular disorders: Muscular dystrophies, diaphragmatic paralysis
- Chest wall abnormalities: Kyphoscoliosis, flail chest
Diagnostic clues: Muscle weakness, progressive difficulty with activities, bulbar symptoms 2.
Table: Key Diagnostic Tests for Dyspnea Categories
| Category | Initial Tests | Advanced Testing |
|---|---|---|
| Cardiac | ECG, BNP, troponin | Echocardiogram, cardiac catheterization |
| Pulmonary | Chest X-ray, spirometry | CT pulmonary angiography, V/Q scan |
| Hematologic/Systemic | CBC, metabolic panel | Carboxyhemoglobin level, lactate levels |
| Neuromuscular | CK, basic neurological exam | EMG/NCS, MRI spine/brain |
5. Diagnostic Testing: Rational Approach to Resource Utilization
Selecting the most appropriate diagnostic tests requires matching clinical suspicion with test characteristics:
- Chest X-ray: First-line imaging for most dyspneic patients; can identify pneumonia, effusions, pneumothorax, congestion 11
- BNP/NT-proBNP: Highly useful for distinguishing cardiac from pulmonary causes (elevated in heart failure) 11
- D-dimer: Reserved for patients with low-moderate probability of PE; high sensitivity but low specificity 11
- Electrocardiogram: Essential for detecting arrhythmias, right heart strain (suggesting PE), or ischemic changes
- Point-of-care ultrasound (POCUS): Rapidly emerging as a bedside tool for differentiating causes:
- B-lines (suggesting pulmonary edema)
- Pleural sliding (absent in pneumothorax)
- Cardiac function (assessment of ejection fraction, pericardial effusion)
- Deep vein thrombosis (often associated with PE) 1
6. Implementing the Systematic Approach to Dyspnea
While most dyspnea stems from physical pathology, psychological factors significantly influence the experience:
- Anxiety and panic disorders can produce terrifying breathlessness despite normal oxygenation
- Dyspnea perception varies substantially based on psychological state, gender, and body weight 17
- Chronic dyspnea often involves complex interactions between physiological limitations and psychological factors
- Treatment approaches should address both physiological impairment and subjective experience when appropriate
7. Conclusion: Integrating Art and Science in Dyspnea Management
Evaluating dyspnea represents both science and art—the science of applying evidence-based diagnostic algorithms, and the art of tailoring the approach to each unique patient. Your visual pyramid framework provides an excellent cognitive aid for ensuring comprehensive differential diagnosis while prioritizing life-threatening conditions.
Remember that definitive treatment depends on identifying the underlying cause, but symptomatic management (including supplemental oxygen, positioning, and sometimes opioids for palliation) should not be overlooked while pursuing diagnosis.
Visual learning resources like your sketch note enhance clinical reasoning by providing mental frameworks that can be recalled during high-stress situations. For a more detailed explanation of this approach, watch our comprehensive video guide “Approach to Dyspnea” on YouTube 🔗