Septic Shock: A Life-Threatening Emergency – What You Need to Know

Sepsis is a medical emergency, and septic shock is its deadliest form. With a mortality rate of ~40%, understanding its diagnosis, pathophysiology, and treatment can save lives. Whether you’re a healthcare professional or a curious reader, this guide breaks down septic shock in an easy-to-digest, blog-friendly format—while keeping it SEO-optimized for visibility.
What is Septic Shock?
Septic shock is a life-threatening condition where an infection triggers a dysregulated immune response, leading to organ failure. It’s defined by:
- The need for vasopressors to maintain blood pressure (MAP ≥65 mmHg).
- Elevated lactate (>2 mmol/L) despite adequate fluids.
Key Takeaway:
- Sepsis ≠ SIRS (old criteria like fever/WBC changes alone aren’t enough).
- Modern diagnosis requires SOFA score ≥2 + confirmed/suspected infection.
How is Septic Shock Diagnosed?
1. SOFA Score (Sequential Organ Failure Assessment)
A SOFA score ≥2 in any system indicates organ dysfunction:
- Respiratory: PaO₂/FiO₂ <300
- Hematologic: Platelets <100k
- Liver: Bilirubin ≥2 mg/dL
- Kidney: Creatinine ≥2 mg/dL
- Neurologic: GCS <13
Pro Tip: *”SOFA ≥2 + infection = sepsis. Add hypotension + high lactate = septic shock.”*
2. Clinical Clues
- Hypotension (MAP <65 mmHg)
- Lactate >2 mmol/L (indicates tissue hypoxia)
- SIRS Criteria (historic but still relevant):
- Temp >38°C or <36°C
- HR >90, RR >20
- WBC >12k or <4k
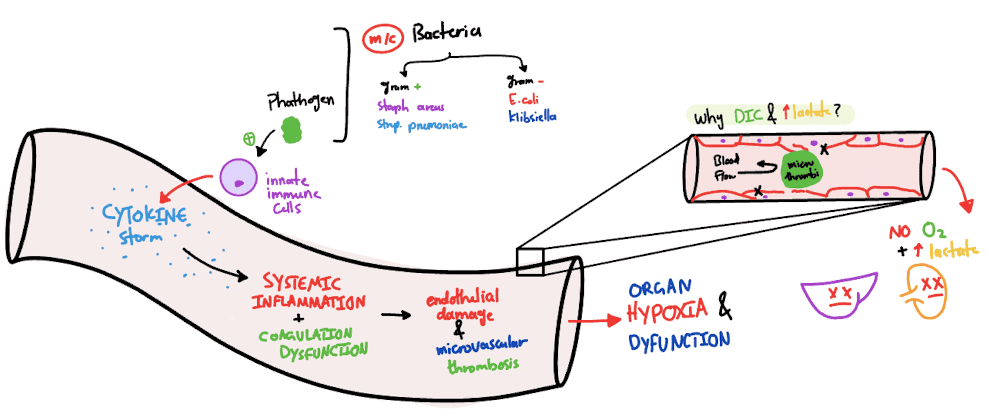
Pathophysiology: Why Does Septic Shock Happen?
Imagine your immune system going haywire—a “cytokine storm” damages blood vessels, causing:
- Massive vasodilation (low blood pressure)
- Microthrombi (tiny clots blocking blood flow)
- Organ failure (ARDS, AKI, liver dysfunction)
Key Mechanism:
- Endotoxins → TNF-α, IL-6 → Nitric Oxide (NO) release → vasodilation + capillary leak.
Failed Therapies?
- Past treatments (like activated protein C) failed because sepsis involves multiple pathways.
Treatment: The Golden Hour Matters
1. Resuscitation (First 6 Hours – EGDT)
- Fluids: 30 mL/kg crystalloid bolus (LR or NS).
- Vasopressors: Norepinephrine is first-line (avoid dopamine—it increases arrhythmias).
- Targets:
- MAP ≥65 mmHg
- Urine output ≥0.5 mL/kg/hr
- CVP 8-12 mmHg (higher if ventilated)
2. Source Control
- Antibiotics:Broad-spectrum within 1 hour (after blood cultures!).
- *Pro Tip: “2 sets of blood cultures (peripheral + central) before antibiotics!”*
- Drainage: Remove infected tissue, abscesses, or devices (e.g., catheters).
3. Adjunctive Therapies
- Steroids: Hydrocortisone (200-300 mg/day) if vasopressor-dependent.
- Blood Sugar Control: Keep glucose <150 mg/dL (but avoid tight control).
- DVT Prophylaxis: LMWH (e.g., enoxaparin) to prevent clots.
Key Evidence & Trials
1. Early Goal-Directed Therapy (EGDT)
- Aggressive 6-hour resuscitation (fluids, vasopressors, ScvO₂ monitoring) reduces mortality.
2. ADRENAL Trial (Steroids in Septic Shock)
- Hydrocortisone shortens vasopressor use but doesn’t improve survival (unless adrenal insufficiency).
3. Antibiotic Duration
- 7-10 days, but reassess at 48-72 hours based on cultures.
Common Pitfalls & Pro Tips
❌ Misdiagnosis: “SIRS alone ≠ sepsis” (e.g., pancreatitis, burns can mimic it).
⚠️ Fluid Overload: Balance resuscitation with CVP/lung sounds (risk of ARDS).
💡 Pro Tip: “Low-dose dopamine doesn’t protect kidneys—avoid it!”